Coronavirus disease 2019 (COVID-19) is a respiratory illness that spreads among people in close contact, primarily through droplets produced when an infected person coughs or sneezes. It can carry with it symptoms of fever, cough, fatigue, and shortness of breath, among others.
The disease — declared a pandemic by the World Health Organization on March 11, 2020 — has spread to every continent except Antarctica and continues to close schools, workplaces, restaurants, and other social spaces as health authorities attempt to slow the spread.
Here are some key statistics to know about COVID-19.
- Background
- Transmission
- Symptoms
- Testing
- Survival Rate, by Age
- Underlying Conditions
- Coronavirus vs. the Flu
- Community Response
1. Coronavirus Background
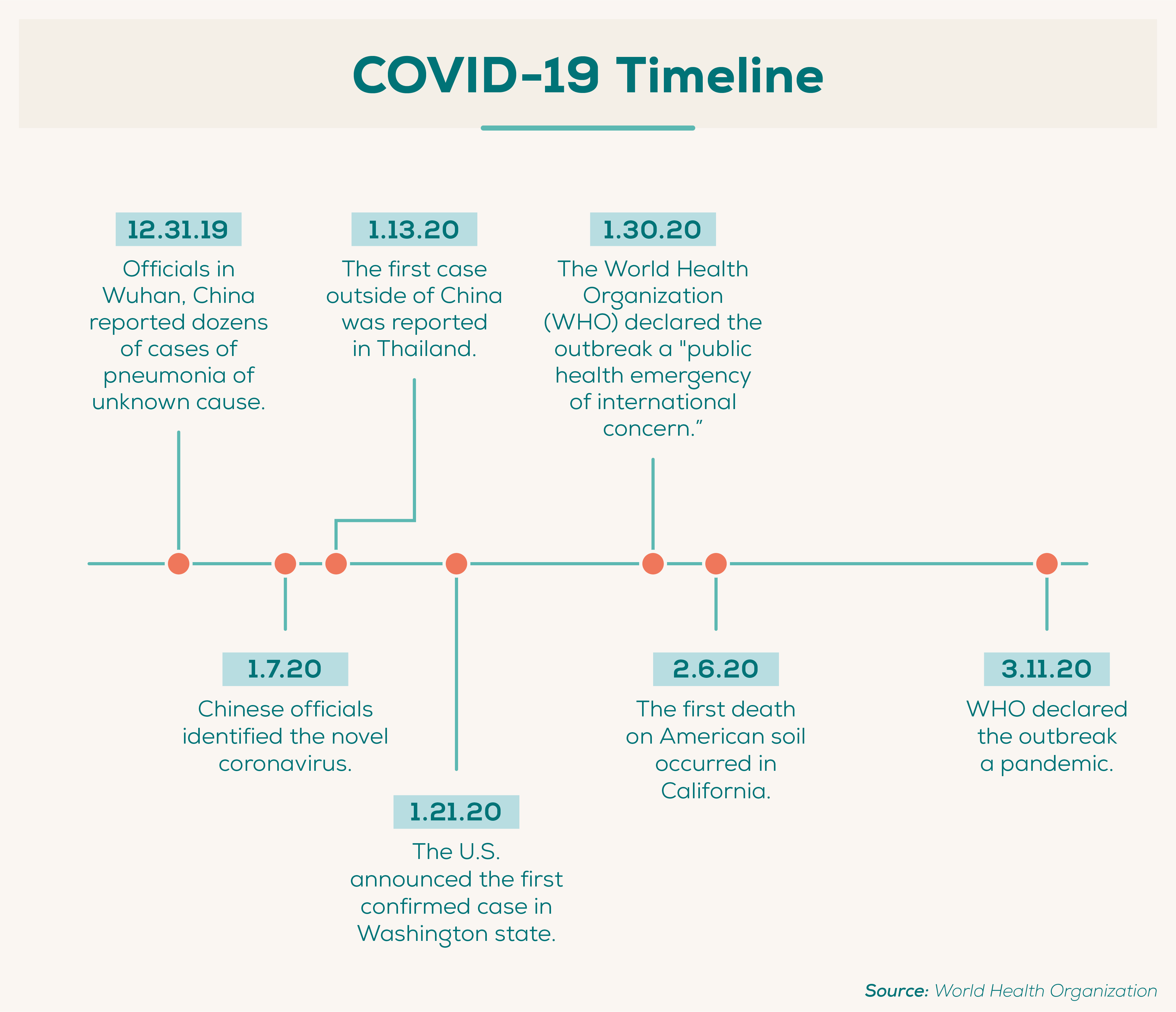
In December 2019, health officials identified several similar cases of pneumonia in Wuhan, the capital of China’s Hubei Province. Chinese health officials identified the cause of the pneumonia as a novel (or new) coronavirus, which was later named SARS-CoV-2.
The virus itself is known as SARS-CoV-2, or Severe Acute Respiratory Syndrome Coronavirus 2, while the disease that results from the virus is called “coronavirus disease 2019” or COVID-19.
- Coronaviruses are a large family of viruses that are common in people and animals, such as camels, cattle, cats, and bats. (CDC)
- Other coronaviruses include MERS-CoV, which was responsible for Middle East Respiratory Syndrome (MERS) first reported in Saudi Arabia in 2012, and SARS-CoV, which was responsible for Severe Acute Respiratory Syndrome (SARS) first reported in Asia in February 2003. (CDC and CDC)
- SARS-CoV-2, like MERS-CoV and SARS-CoV, originated in bats. (CDC)
- Four types of human coronaviruses found around the world account for 10–30% of upper respiratory tract infections in adults. (Journal of the American Medical Association)
- The World Health Organization declared the outbreak a “public health emergency of international concern” on January 30, 2020, and a pandemic on March 11, 2020. (WHO and WHO)
2. Coronavirus Transmission
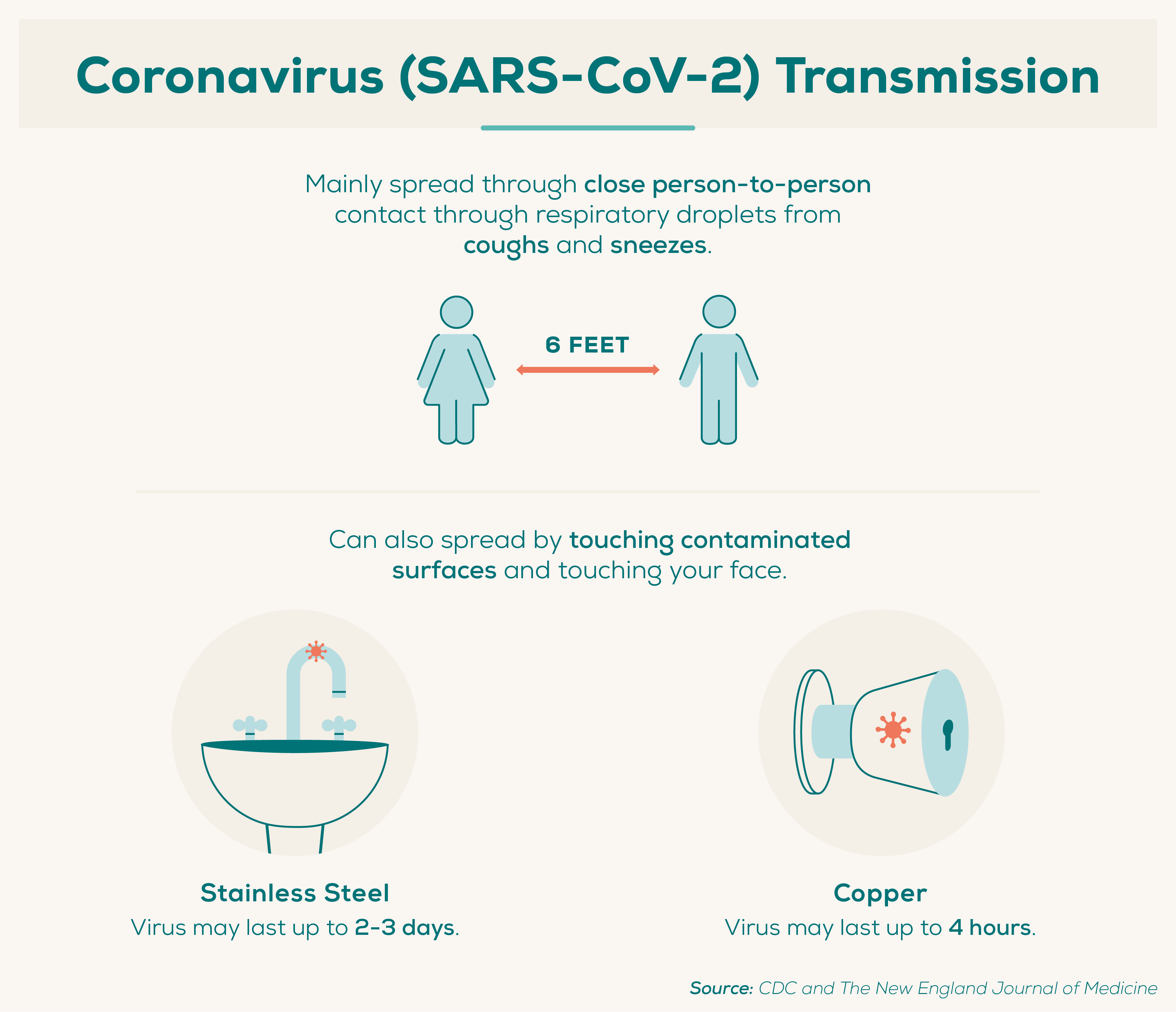
According to the Centers for Disease Control and Prevention, the virus is thought to spread mainly among people in close contact with one another (six feet or less) through droplets produced when an infected person coughs or sneezes. The droplets can land in people’s mouths or noses or be inhaled.
The virus may also spread when people touch contaminated surfaces and later touch their mouths, noses, or eyes.
Research suggests that people are most contagious when they show the most symptoms, but it may be possible for someone who doesn’t show any symptoms to spread the virus.
- Coronavirus mainly spreads through respiratory droplets (produced by coughing or sneezing) among people in close proximity to one another (within 6 feet). (CDC)
- On average, each infected person spreads the infection to another two people. (The New England Journal of Medicine)
- Coronavirus may last in droplets in the air for up to 3 hours. (The New England Journal of Medicine)
- Coronavirus may last on copper for up to 4 hours. (The New England Journal of Medicine)
- Coronavirus may last on stainless steel for 2–3 days. (The New England Journal of Medicine)
- Human coronaviruses on surfaces can be inactivated within a minute using disinfectants with 62–71% ethanol, 0.5% hydrogen peroxide, or 0.1% sodium hypochlorite. (Journal of Hospital Infection)
3. COVID-19 Symptoms
- COVID-19 symptoms may appear 2–14 days after exposure. (CDC, based on the incubation period of MERS-CoV)
- The median incubation period (time between exposure and first symptoms) for COVID-19 is 5.1 days. (Annals of Internal Medicine, based on 181 cases from China and other countries prior to February 24, 2020)
- 97.5% of people who develop symptoms will do so within 11.5 days of being infected. (Annals of Internal Medicine, based on 181 cases from China and other countries prior to Feb. 24)
- COVID-19 symptoms may last about 2 weeks in mild cases and 3–6 weeks in severe or critical cases. (WHO)
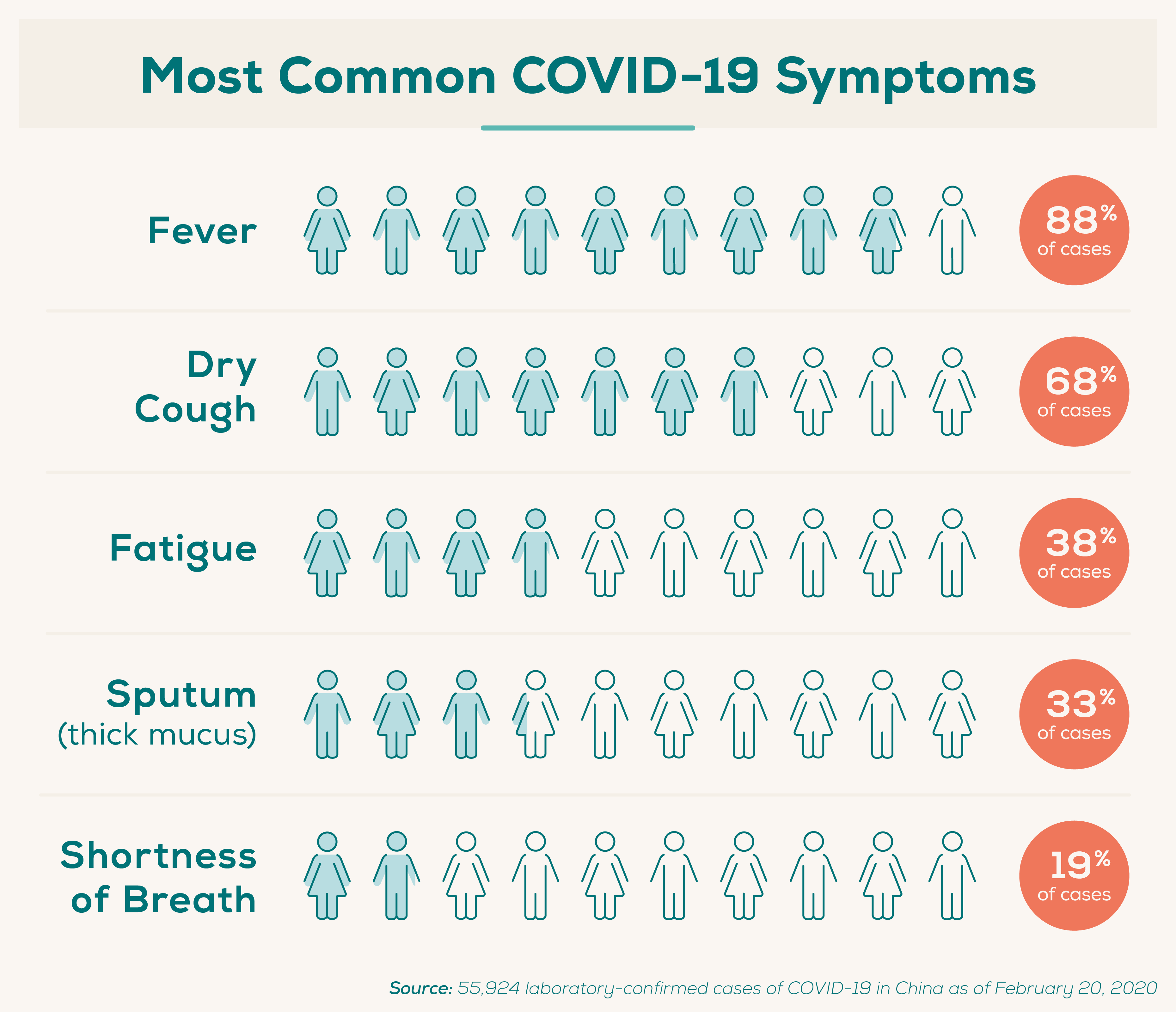
Of 55,924 laboratory-confirmed cases of COVID-19 in China as of February 20, 2020 (WHO):
- 87.9% experienced fever.
- 67.7% experienced a dry cough.
- 38.1% experienced fatigue.
- 33.4% produced sputum (thick mucus).
- 18.6% experienced shortness of breath.
In the same study, there were numerous less common symptoms:
- 14.8% experienced muscle or joint pain.
- 13.9% experienced a sore throat.
- 13.6% had a headache.
- 11.4% had chills.
- 5% experienced nausea or vomiting.
- 4.8% experienced nasal congestion.
- 3.7% experienced diarrhea.
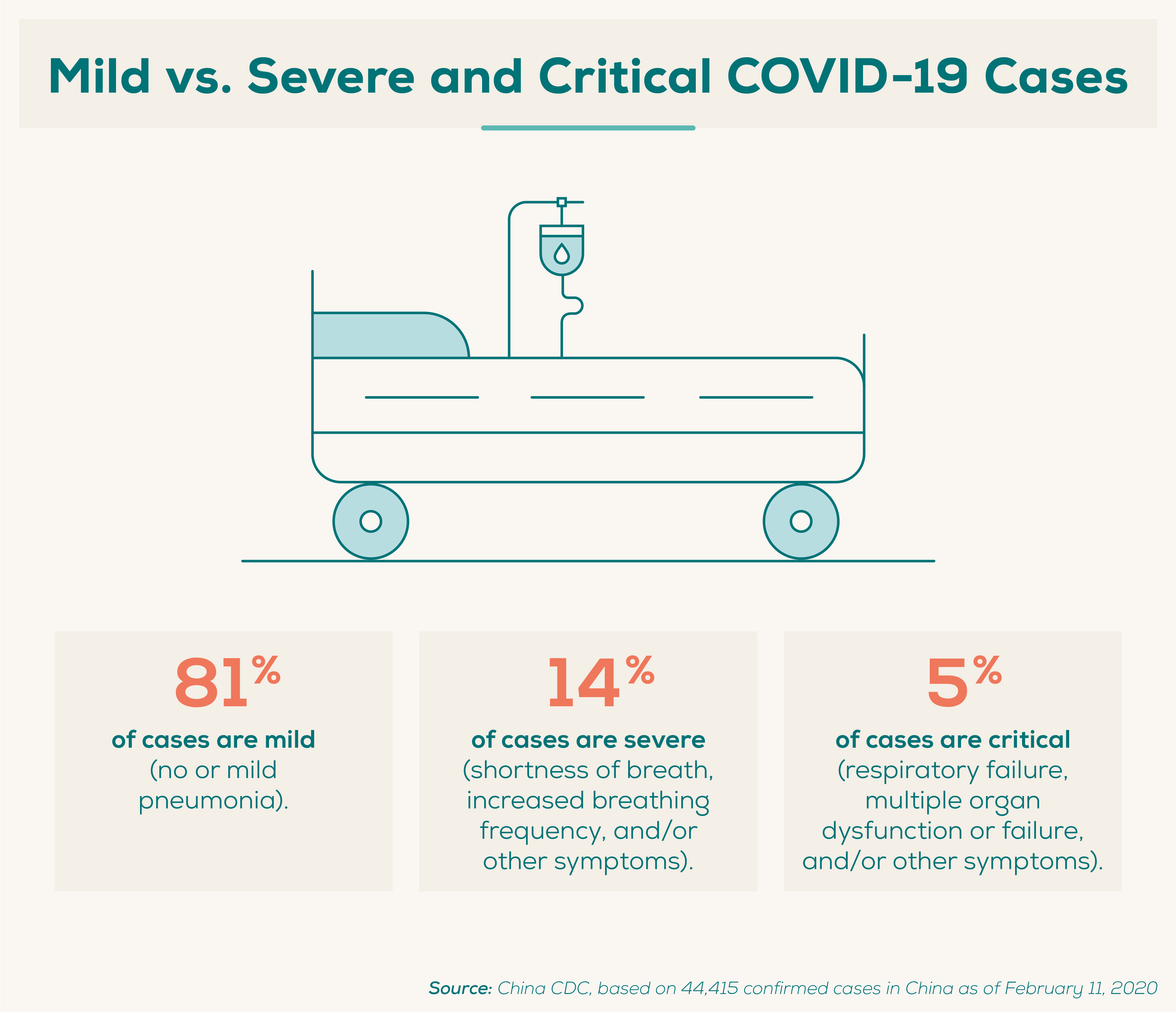
Of 44,415 confirmed cases in China as of February 11, 2020 (China CDC):
- 80.9% of cases were mild, involving mild or no pneumonia.
- 13.8% of cases were severe, involving shortness of breath, increased respiratory frequency, decreased blood oxygen saturation, and/or increased lung infiltrates.
- 4.7% of COVID-19 cases were critical, involving respiratory failure, septic shock, and/or multiple organ dysfunction or failure.
4. COVID-19 Testing
Testing in the U.S. has lagged behind other countries for a number of reasons. Various government policies and testing errors prevented the involvement of private labs early on in the outbreak and delayed the widespread availability of the tests. That left public health experts largely unaware of the extent of the outbreak.
At the same time, until late February — more than a month after the first confirmed COVID-19 case in the U.S. — testing was limited to those who had traveled to China or who had been exposed to someone known to be infected. That meant that many people who showed symptoms but did not meet the criteria were turned away without testing.
Health experts have stressed the need to test as many people as possible so that those with COVID-19 know if they have it and can take appropriate action; this will also help health experts gain a clear picture of the outbreak in order to make informed policy decisions.
It’s especially important for frontline healthcare workers to have access to testing since they play a critical role in caring for sick patients but also face a high risk of exposure to COVID-19. Everlywell has partnered with hospitals, clinics, nursing homes, and government agencies to supply testing to thousands of healthcare workers, seniors, and high-risk patients.
- On March 4, 2020 — a week after the first confirmed community transmission case in the U.S. — the U.S. had tested fewer than 1,000 people total. (The COVID Tracking Project)
- At that same point (March 4, 2020), South Korea, which was quick to mobilize testing, had tested almost 150,000 people and was testing more than 10,000 people per day (KCDC)
- The United States, as of April 16, 2020, had tested only 1% of its population. (The COVID Tracking Project and U.S. Census Bureau)
- Canada, as of April 16, 2020, had tested 1.3% of its population. (Public Health Agency of Canada and World Population Review)
- South Korea, as of April 16, 2020, had tested 1.2% of its population. (KCDC and The World Bank)
- Norway, as of April 15, 2020, had tested 2.5% of its population. (NIPH and World Population Review)
- Coronavirus tests typically swab the back of the nose. (Everlywell)
- The Everlywell test initially launched with 30,000 kits, with the kits going to those who need them the most: healthcare workers, seniors, and high-risk patients. (Everlywell)
- The Everlywell test is available at cost (meaning no profit to Everlywell). See a complete breakdown of the costs that go into providing the test. (Everlywell)
- Everlywell tests are processed within 48 hours of lab receipt. (Everlywell)
5. COVID-19 Survival Rate
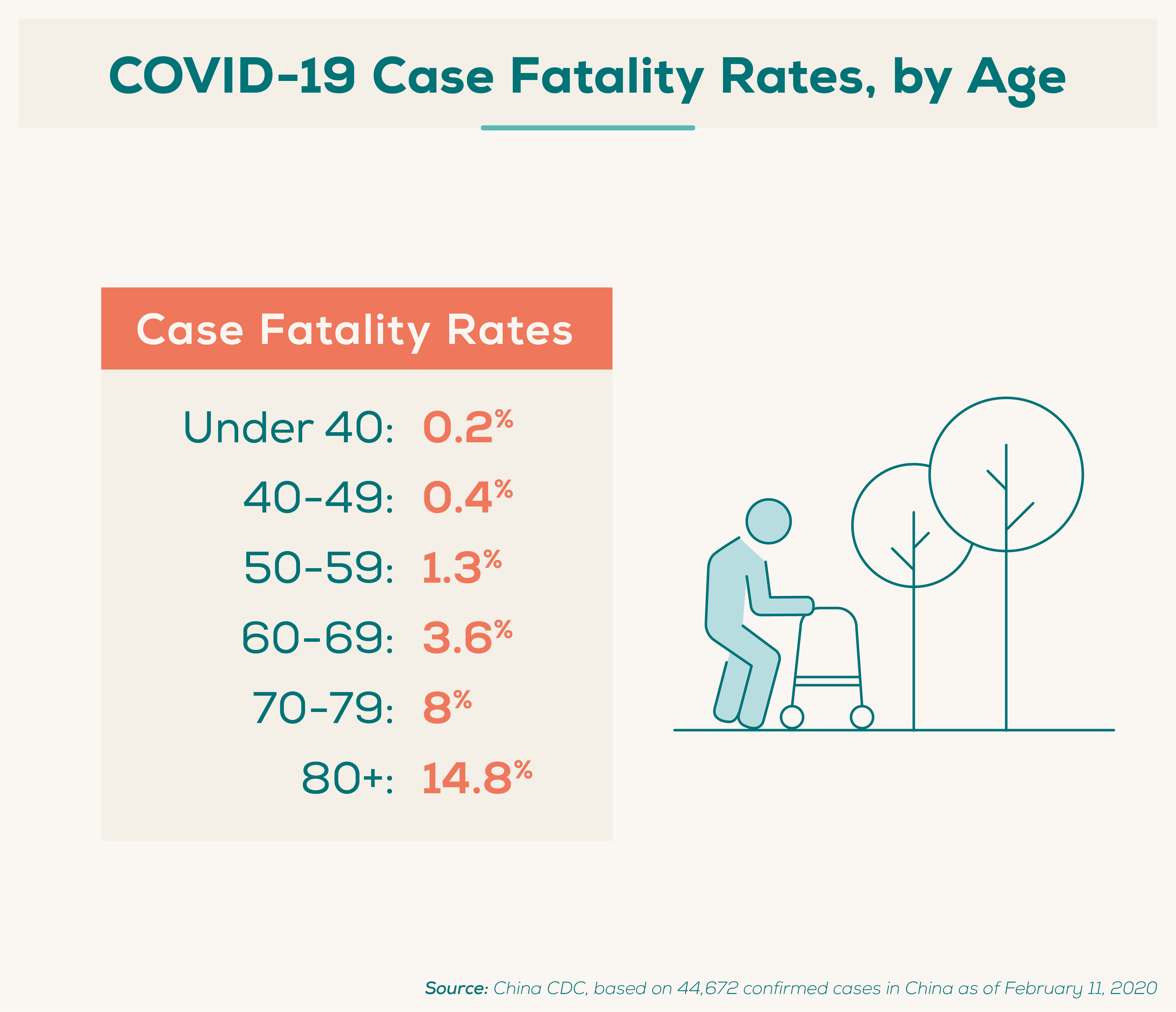
Researchers often look at the case fatality rate, which is the proportion of people who die from a disease of those who have been diagnosed with it. The case fatality rate can vary substantially over time depending on the specific characteristics of those infected.
Case fatality rates for COVID-19 have been reported to be as low as less than 2%. The case fatality rate may even be less than 1% if the number of asymptomatic or cases with minimal symptoms is significantly higher than the number of reported cases, according to The New England Journal of Medicine.
Of 44,672 confirmed COVID-19 cases in China as of February 11, 2020 (China CDC):
- The case fatality rate for ages 10–19 was 0.2%.
- The case fatality rate for ages 20–29 was 0.2%.
- The case fatality rate for ages 30–39 was 0.2%.
- The case fatality rate for ages 40–49 was 0.4%.
- The case fatality rate for ages 50–59 was 1.3%.
- The case fatality rate for ages 60–69 was 3.6%.
- The case fatality rate for ages 70–79 was 8%.
- The case fatality rate for ages 80+ was 14.8%.
U.S. data of 2,449 COVID-19 cases from February 12, 2020, through March 16, 2020, showed (CDC):
- The case fatality rate for ages 20–44 was 0.1–0.2%.
- The case fatality rate for ages 45–54 was 0.5–0.8%.
- The case fatality rate for ages 55–64 was 1.4–2.6%.
- The case fatality rate for ages 65–74 was 2.7–4.9%.
- The case fatality rate for ages 75–84 was 4.3–10.5%.
- The case fatality rate for ages 85+ was 10.4–27.3%.
Meanwhile U.S. data of 1,482 COVID-19 cases from March 1, 2020, through March 28, 2020, showed that younger adults are also at risk of being hospitalized for COVID-19 (CDC):
- 0.4% of hospitalized patients were younger than 18.
- 24.7% of hospitalized patients were 18–49.
- 31.1% of hospitalized patients were 50–64.
- 43.4% of hospitalized patients were 65 or older.
6. Underlying Conditions
In that same study of 44,672 confirmed COVID-19 cases in China as of February 11, 2020 (China CDC):
- 10.5% of those with cardiovascular disease who were diagnosed with COVID-19 died.
- 7.3% of those with diabetes who were diagnosed with COVID-19 died.
- 6.3% of those with chronic respiratory disease who were diagnosed with COVID-19 died.
- 6% of those with hypertension who were diagnosed with COVID-19 died.
- 5.6% of those with cancer who were diagnosed with COVID-19 died.
7. COVID-19 vs. the Flu
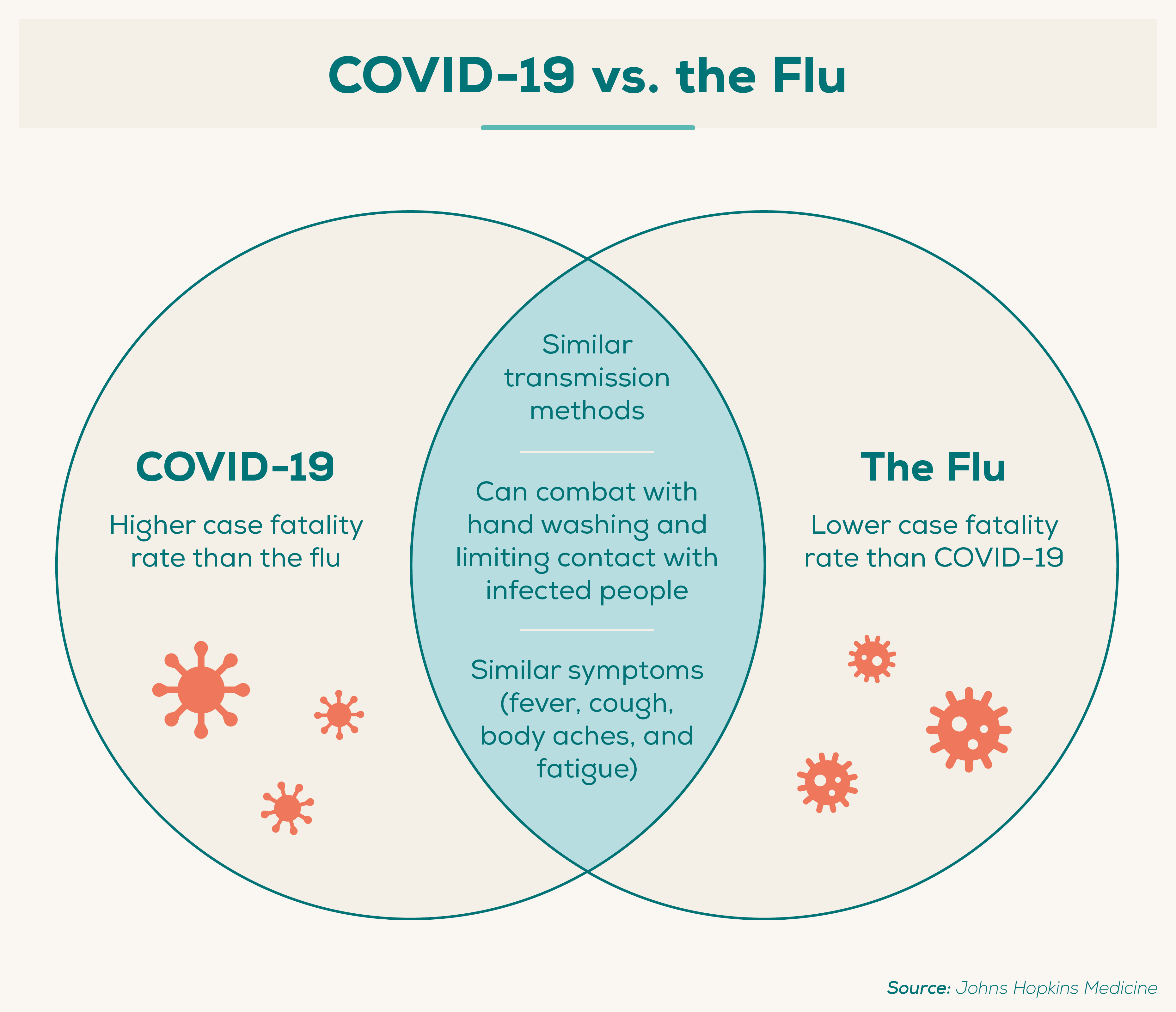
COVID-19 and influenza, or “the flu,” are both infectious respiratory illnesses that may carry many of the same symptoms: fever, cough, and fatigue. Both may be spread via the same methods and can be prevented by thorough hand washing and social distancing.
The two illnesses differ in their case fatality rates and overall number of infections (though, of course, the flu isn’t new, so the case counts are higher). Another significant difference lies in the fact that there is currently no vaccine for COVID-19, though one exists for the flu.
- The case fatality rate for the flu is approximately 0.1%, which is much lower than any estimate of the case fatality rate for COVID-19. (The New England Journal of Medicine)
- There are 9.3–45 million flu cases in the U.S. every year and about 1 billion cases worldwide, which is currently higher than COVID-19 cases. (Johns Hopkins University)
- There are 12,000–61,000 flu deaths in the U.S. per year and 291,000–646,000 flu deaths worldwide, which is currently higher than COVID-19 deaths. (Johns Hopkins University)
8. Community Response
The philanthropic response to COVID-19 has been enormous, with organizations and individuals pitching in billions of dollars to help those affected by the pandemic.
- $7.5 billion in grants have been earmarked for the coronavirus outbreak, as of April 17, 2020. (Candid)
- Most grants have gone toward recipients focused on medical services and disaster relief, but $528 million has gone to education, and $691 million has gone to food aid, as of April 17, 2020. (Candid)
- In contrast, philanthropic funding totaled $363 million in the 6 months after the Ebola outbreak in 2014. (Candid)
- Philanthropic funding totaled less than $400 million for Hurricane Harvey and less than $200 million each for the Australian bushfires and Hurricanes Irma, Maria, and Dorian. (Candid)
- Everlywell funded a $1 million Development Incentive Program to increase capacity for COVID-19 testing (Everlywell)
- Everlywell has provided thousands of tests to frontline healthcare workers, seniors, and high risk patients nationwide. (Everlywell)
It’s important to do your part to promote your own safety and the safety of others during the COVID-19 pandemic.
If you’re experiencing symptoms such as fever, cough, or shortness of breath; you’ve been in close contact with someone confirmed or suspected to have COVID-19; you’ve been to certain countries where widespread community transmission has been reported; or you’ve been in community areas where COVID-19 cases have been reported, you should seek testing.
The Everlywell COVID-19 Test Home Collection Kit provides results within 48 hours after the lab receives the sample—and is available at cost (no profit to Everlywell).
Share This Post















